
Summary
Calcinosis cutis is an uncommon condition marked by calcium buildup in the skin and subcutaneous tissues. Calcinosis cutis can range in intensity from little nodules in one area of the body to huge, crippling lesions affecting a vast portion of the body.[1] Five kinds of the condition are typically distinguished: calciphylaxis, idiopathic calcification, iatrogenic calcification, dystrophic calcification, and metastatic calcification.[2]
| Calcinosis cutis | |
|---|---|
| Other names | Cutaneous calcification |
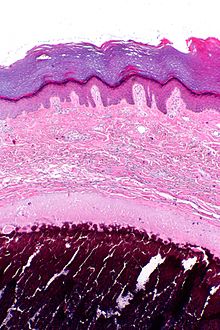 | |
| Micrograph of calcinosis cutis. The calcification is purple (bottom of image). H&E stain. | |
| Specialty | Dermatology |
Tumors, inflammation, varicose veins, infections, connective tissue disease, hyperphosphatemia, and hypercalcemia can all lead to calcinosis. Systemic sclerosis is linked to calcineuris cutis.[3] Calcinosis is seen in Limited Cutaneous Systemic Sclerosis, also known as CREST syndrome (the "C" in CREST).[4]
Signs and symptoms edit
Lesions might be more severe and widespread, or they can develop gradually and show no symptoms. The nodules may cause pain and hinder function in addition to having a variety of sizes and shapes. The underlying condition determines the localization of the lesions in dystrophic calcification. The elbows, fingers, knees, and forearms are the most often affected regions in people with systemic sclerosis. Elbows, knees, and regions of prior inflammatory lesions in dermatomyositis are affected by calcification. Lupus erythematosus affects the limbs, buttocks, area beneath lupus lesions, and periarticular areas. Periarticular lesions are found in metastatic calcification. In tumoral calcinosis, the lesions are found around joints, but in idiopathic calcification, the lesions are found on children's faces as subepidermal calcified nodules. In iatrogenic calcification, the calcification is found at venipuncture sites.[3]
Causes edit
Calcinosis may result from a variety of causes such as:[3]
- Trauma to the region
- Inflammation (bug bites, acne)
- Varicose veins
- Infections
- Tumors (malignant or benign)
- Diseases of connective tissue
- Hypercalcemia
- Hyperphosphatemia
Calcinosis cutis is associated with systemic sclerosis.[3]
Diagnosis edit
Classification edit
Calcinosis cutis may be divided into the following types:[5]: 527–530
Dystrophic calcinosis cutis edit
Dystrophic calcinosis cutis is the most prevalent kind of calcification on the skin.[2] The ectopic calcified mass usually consists of amorphous calcium phosphate and hydroxyapatite.[6] Dystrophic calcification is linked to a number of illnesses, such as infections, hereditary diseases, cutaneous neoplasms, and connective tissue diseases.[7] The clinical manifestation can be as minor as an accidental radiography imaging finding or as severe as subcutaneous nodules or plaques.[8]
Metastatic calcinosis cutis edit
Metastatic calcinosis cutis is the consequence of calcium salts precipitating in normal tissue due to an underlying abnormality in the metabolism of phosphate and/or calcium.[2] Metastatic calcification can result from any systemic condition raising serum calcium and/or phosphate levels. Chronic renal failure is the most frequent underlying cause.[9]
Iatrogenic calcinosis cutis edit
Iatrogenic calcinosis cutis is characterized by firm nodules in the subcutis or dermis, which are caused by calcium salts precipitating quickly in the skin.[9] This occurrence typically manifests as a warm, sensitive swelling at the site of venipuncture,[2] and it most frequently happens following the extravasation of intravenous calcium chloride, calcium gluconate, or phosphate-containing solutions.[10] Iatrogenic calcification, which manifests as soft yellow-white epidermal plaques,[2] has also been linked to calcium salt exposure via electroencephalography or electromyographic electrode compounds.[11]
Traumatic calcinosis cutis edit
Traumatic calcinosis cutis is a cutaneous condition characterized by calcification of the skin resulting from the deposition of calcium and phosphorus often resulting from occupational exposure, as in cases reported in oil-field workers and coal miners.[12]: 528
Idiopathic calcinosis cutis edit
Skin calcification that is not linked to a systemic illness or an underlying tissue injury is referred to as idiopathic calcification.[2] Most often, the calcification is restricted to a single general location, yet there has been one case of calcinosis cutis that is exceptionally broad.[13]
Idiopathic scrotal calcinosis edit
Idiopathic scrotal calcinosis is a cutaneous condition characterized by calcification of the skin resulting from the deposition of calcium and phosphorus occurring on the scrotum.[14]: 528 However, the levels of calcium and phosphate in the blood are normal.[15] Idiopathic scrotal calcinosis typically affects young males, with an onset between adolescence and early adulthood.[15] The scrotal calcinosis appears, without any symptoms, as yellowish nodules that range in size from 1 mm to several centimeters.[16]
Subepidermal calcified nodule edit
Subepidermal calcified nodule is characterized by calcification of the skin resulting from the deposition of calcium and phosphorus, occurring most frequently as one or a few skin lesions on the scalp or face of children.[17]: 528
Tumoral calcinosis edit
Tumoral calcinosis is distinguished by the accumulation of calcific masses surrounding the main joints. It mainly affects teens who are otherwise in good health. Joint function may be hampered by the subcutaneous or intramuscular calcified deposits.[2]
Osteoma cutis edit
Osteoma cutis is a cutaneous condition characterized by the presence of bone within the skin in the absence of a preexisting or associated lesion.[18]: 529 Osteoma cutis often manifests as solid, varying-sized, skin-colored subcutaneous nodules.[19]
Treatment edit
Diltiazem, a calcium channel blocker, has been a mainstay of medical treatment for calcinosis cutis.[1] It is thought to work by modifying intracellular calcium levels, which reduces the capacity for the production and crystallization of calcium nidus.[20]
Colchicine is an antimicrotubule drug with anti-inflammatory properties that has been used for gouty arthritis treatment for a long time.[1] Calcinosis cutis inflammation brought on by a foreign body-like response aggravates the illness's symptoms.[21] Colchicine, therefore, has been used to treat calcinosis cutis, albeit with varying degrees of success.[1]
Gallery edit
-
Calcinosis cutis in a dog with Cushing's syndrome
-
Histopathology of calcinosis cutis in human tissue
See also edit
References edit
- ^ a b c d Gutierrez Jr, Albert; Wetter, David A. (2012). "Calcinosis cutis in autoimmune connective tissue diseases: Calcinosis cutis and connective tissue disease". Dermatologic Therapy. 25 (2): 195–206. doi:10.1111/j.1529-8019.2012.01492.x. PMID 22741938.
- ^ a b c d e f g Reiter, Nadine; El-Shabrawi, Laila; Leinweber, Bernd; Berghold, Andrea; Aberer, Elisabeth (2011). "Calcinosis cutis". Journal of the American Academy of Dermatology. 65 (1): 1–12. doi:10.1016/j.jaad.2010.08.038. PMID 21679810.
- ^ a b c d Le, Cuong; Bedocs, Paul M. (2023-07-10). "Calcinosis Cutis". StatPearls Publishing. PMID 28846311. Retrieved 2024-02-28.
- ^ "CREST syndrome: MedlinePlus Medical Encyclopedia Image". medlineplus.gov. Retrieved 2023-02-12.
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ Wang, Wen-Jen (1988-11-01). "Calcinosis Cutis in Juvenile Dermatomyositis: Remarkable Response to Aluminum Hydroxide Therapy". Archives of Dermatology. 124 (11): 1721. doi:10.1001/archderm.1988.01670110077022. ISSN 0003-987X. PMID 3178257.
- ^ Walsh, John S; Fairley, Janet A (1995). "Calcifying disorders of the skin". Journal of the American Academy of Dermatology. 33 (5): 693–706. doi:10.1016/0190-9622(95)91803-5. PMID 7593766.
- ^ Boulman, Nina; Slobodin, Gleb; Rozenbaum, Michael; Rosner, Itzhak (2005). "Calcinosis in Rheumatic Diseases". Seminars in Arthritis and Rheumatism. 34 (6). Elsevier BV: 805–812. doi:10.1016/j.semarthrit.2005.01.016. ISSN 0049-0172. PMID 15942915.
- ^ a b "UpToDate". UpToDate. Retrieved 2024-02-29.
- ^ Amati, C.; Pesce, V.; Armenio, A.; Solarino, G.; Moretti, B. (2015-04-08). "Tumoral calcinosis of the hand". Journal of Surgical Case Reports. 2015 (4). Oxford University Press (OUP): rjv036. doi:10.1093/jscr/rjv036. hdl:11586/171759. ISSN 2042-8812. PMC 4390718. PMID 25858267.
- ^ Touart, Diane M.; Sau, Purnima (1998). "Cutaneous deposition diseases. Part II". Journal of the American Academy of Dermatology. 39 (4). Elsevier BV: 527–546. doi:10.1016/s0190-9622(98)70001-5. ISSN 0190-9622. PMID 9777759.
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ Guermazi, Ali; Grigoryan, Mikayel; Cordoliani, Florence; Kérob, Delphine (2006-12-21). "Unusually diffuse idiopathic calcinosis cutis". Clinical Rheumatology. 26 (2): 268–270. doi:10.1007/s10067-005-0135-8. ISSN 0770-3198. PMID 16416033.
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ a b Grenader, Tal; Shavit, Linda (Aug 18, 2011). "Scrotal Calcinosis". New England Journal of Medicine. 365 (7): 647. doi:10.1056/NEJMicm1013803. PMID 21848465.
- ^ Khallouk A, Yazami OE, Mellas S, Tazi MF, El Fassi J, Farih MH (2011). "Idiopathic scrotal calcinosis: a non-elucidated pathogenesis and its surgical treatment". Reviews in Urology. 13 (2): 95–7. PMC 3176555. PMID 21935341.
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ Niebel, Dennis; Poortinga, Sietske; Wenzel, rg (2020-09-22). "Osteoma Cutis and Calcinosis Cutis: "Similar but Different"". The Journal of Clinical and Aesthetic Dermatology. 13 (11). Matrix Medical Communications: 28–31. PMC 7716738. PMID 33282099.
- ^ Fuchs, D; Fruchter, L; Fishel, B; Holtzman, M; Yaron, M (December 1986). "Colchicine suppression of local inflammation due to calcinosis in dermatomyositis and progressive systemic sclerosis". Clinical Rheumatology. 5 (4): 527–530. PMID 3816102.
Further reading edit
- Reiter, Nadine; El-Shabrawi, Laila; Leinweber, Bernd; Berghold, Andrea; Aberer, Elisabeth (2011). "Calcinosis cutis". Journal of the American Academy of Dermatology. 65 (1): 15–22. doi:10.1016/j.jaad.2010.08.039. PMID 21679811.
- Róbert, Lili; Kiss, Norbert; Medvecz, Márta; Kuroli, Enikő; Sárdy, Miklós; Hidvégi, Bernadett (2020). "Epidemiology and treatment of calcinosis cutis: 13 years of experience". Indian Journal of Dermatology. 65 (2). Medknow: 105–111. doi:10.4103/ijd.ijd_527_18. ISSN 0019-5154. PMC 7059479. PMID 32180595.
External links edit
- DermNet
- WebMD


