
Summary
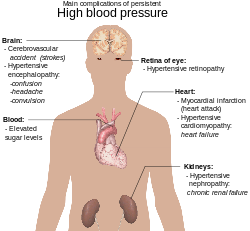
Complications of hypertension are clinical outcomes that result from persistent elevation of blood pressure.[1] Hypertension is a risk factor for all clinical manifestations of atherosclerosis since it is a risk factor for atherosclerosis itself.[2][3][4][5][6][7] It is an independent predisposing factor for heart failure,[8][9] coronary artery disease,[10][11] stroke,[1] kidney disease,[12][13][14] and peripheral arterial disease.[15][16] It is the most important risk factor for cardiovascular morbidity and mortality, in industrialized countries.[17]
Complications affecting the heart edit
Hypertensive heart disease is the result of structural and functional adaptations[18] leading to left ventricular hypertrophy,[19][20][21] diastolic dysfunction,[18][20] CHF (Congestive Heart Failure), abnormalities of blood flow due to atherosclerotic coronary artery disease[18] and microvascular disease,[10][19] and cardiac arrhythmias.[19] Individuals with left ventricular hypertrophy are at increased risk for, stroke,[22] CHF,[22] and sudden death.[22] Aggressive control of hypertension can regress or reverse left ventricular hypertrophy and reduce the risk of cardiovascular disease.[23] [24][25][26] left ventricular hypertrophy are seen in 25% of the hypertensive patients and can easily be diagnosed by using echocardiography.[27] Underlying mechanisms of hypertensive left ventricular hypertrophy are of 2 types: firstly, mechanical (mainly leading to myocyte hypertrophy) and secondly, neuro-hormonal(mainly resulting in a fibroblastic proliferation).[27]
Abnormalities of diastolic function, ranging from asymptomatic heart disease[28][29][30] to overt heart failure,[31][32] are common in hypertensive patients. Patients with diastolic heart failure have a preserved ejection fraction, which is a measure of systolic function.[33][34] Diastolic dysfunction is an early consequence of hypertension-related heart disease and is exacerbated by left ventricular hypertrophy[20][34] and ischemia.
Complications affecting the brain edit
Hypertension is an important risk factor for brain infarction and hemorrhage.[1][10][35][36][37][38][39][40][excessive citations] Approximately 85% of strokes are due to infarction and the remainder are due to hemorrhage, either intracerebral hemorrhage or subarachnoid hemorrhage.[41] The incidence of stroke rises progressively with increasing blood pressure levels, particularly systolic blood pressure in individuals >65 years. Treatment of hypertension convincingly decreases the incidence of both ischemic and hemorrhagic strokes.[41]
Hypertension is also associated with impaired cognition in an aging population.[42][43][44][45] Hypertension-related cognitive impairment and dementia may be a consequence of a single infarct due to occlusion of a "strategic" larger vessel[46][47] or multiple lacunar infarcts due to occlusive small vessel disease resulting in subcortical white matter ischemia.[43][45][48] Several clinical trials suggest that antihypertensive therapy has a beneficial effect on cognitive function, although this remains an active area of investigation.[49][50][51]
Cerebral blood flow remains unchanged over a wide range of arterial pressures (mean arterial pressure of 50–150 mmHg) through a process termed autoregulation of blood flow.[52] Signs and symptoms of hypertensive encephalopathy may include severe headache, nausea and vomiting (often of a projectile nature), focal neurologic signs, and alterations in mental status. Untreated, hypertensive encephalopathy may progress to stupor, coma, seizures, and death within hours.[53][54][55][56] It is important to distinguish hypertensive encephalopathy from other neurologic syndromes that may be associated with hypertension, e.g., cerebral ischemia, hemorrhagic or thrombotic stroke, seizure disorder, mass lesions, pseudotumor cerebri, delirium tremens, meningitis, acute intermittent porphyria, traumatic or chemical injury to the brain, and uremic encephalopathy.[41]
Complications affecting the eye edit
Hypertensive retinopathy is a condition characterized by a spectrum of retinal vascular signs in people with elevated blood pressure.[57] It was first described by Liebreich in 1859.[58] The retinal circulation undergoes a series of pathophysiological changes in response to elevated blood pressure.[59] In the initial, vasoconstrictive stage, there is vasospasm and an increase in retinal arteriolar tone owing to local autoregulatory mechanisms. This stage is seen clinically as a generalized narrowing of the retinal arterioles. Persistently elevated blood pressure leads to intimal thickening, hyperplasia of the media wall, and hyaline degeneration in the subsequent, sclerotic, stage. This stage corresponds to more severe generalized and focal areas of arteriolar narrowing, changes in the arteriolar and venular junctions, and alterations in the arteriolar light reflex (i.e., widening and accentuation of the central light reflex, or "copper wiring").[60]
This is followed by an exudative stage, in which there is disruption of the blood–retina barrier, necrosis of the smooth muscles and endothelial cells, exudation of blood and lipids, and retinal ischemia. These changes are manifested in the retina as microaneurysms, hemorrhages, hard exudates, and cotton-wool spots. Swelling of the optic disk may occur at this time and usually indicates severely elevated blood pressure (i.e., malignant hypertension). Because better methods for the control of blood pressure are now available in the general population, malignant hypertension is rarely seen. In contrast, other retinal vascular complications of hypertension, such as macroaneurysms and branch-vein occlusions, are not uncommon in patients with chronically elevated blood pressure. These stages of hypertensive retinopathy however, may not be sequential.[59][61] For example, signs of retinopathy that reflect the exudative stage, such as retinal hemorrhage or microaneurysm, may be seen in eyes that do not have features of the sclerotic stage,[59] The exudative signs are nonspecific, since they are seen in diabetes and other conditions.[citation needed]
Complications affecting the kidneys edit
Hypertension is a risk factor for chronic kidney disease and end-stage kidney disease (ESKD).[62][63][64][65][66][67][68][excessive citations] Kidney risk appears to be more closely related to systolic than to diastolic blood pressure,[69][70] and black men are at greater risk than white men for developing ESRD at every level of blood pressure.[71][72][73][74][75]
The atherosclerotic, hypertension-related vascular lesions in the kidney primarily affect the preglomerular arterioles,[69][76][77] resulting in ischemic changes in the glomeruli and postglomerular structures.[41] Glomerular injury may also be a consequence of direct damage to the glomerular capillaries due to glomerular hyperperfusion. Glomerular pathology progresses to glomerulosclerosis,[78][79] and eventually the kidney tubules may also become ischemic and gradually atrophic. The kidney lesion associated with malignant hypertension consists of fibrinoid necrosis of the afferent arterioles,[80][81][82][83][84][85][86][excessive citations] sometimes extending into the glomerulus, and may result in focal necrosis of the glomerular tuft.[82][87][88]
Clinically, macroalbuminuria (a random urine albumin/creatinine ratio > 300 mg/g) or microalbuminuria (a random urine albumin/creatinine ratio 30–300 mg/g) are early markers of kidney injury. These are also risk factors for kidney disease progression and for cardiovascular disease.[41]
Complications associated to diabetes and hypertension edit
Diabetes has several complications of which one is hypertension or high blood pressure. Data indicate that at least 60-80 percent of individuals whom develop diabetes will eventually develop high blood pressure. The high blood pressure is gradual at early stages and may take at least 10–15 years to fully develop. Besides diabetes, other factors that may also increase high blood pressure include obesity, insulin resistance and high cholesterol levels. In general, fewer than 25 percent of diabetics have good control of their blood pressure. The presence of high blood pressure in diabetes is associated with a 4 fold increase in death chiefly from heart disease and strokes.[89] It has also been shown in recent epidemiological studies that variability of blood pressure, independent of mean blood pressure level, contributes to microvascular and macrovascular complications[90] in those with diabetes, including heart failure.[91] These variability associations may be especially deleterious in persons with either particularly high or particularly low blood pressures.[92]
The chief reason why people with diabetes develop high blood pressure is hardening of the arteries. Diabetes tends to speed up the process of atherosclerosis. The other fact about diabetes is that it affects both large and small blood vessels in the body. Over time, blood vessels become clogged with fatty depots, become non-compliant and lose their elasticity. The process of atherosclerosis is a lot faster in diabetic individuals whom do not have good control of their blood sugars. The high blood pressure eventually leads to heart failure, strokes, heart attacks, blindness, kidney failure, loss of libido and poor circulation of blood in the legs. When the blood supply to the feet is compromised, the chances of infections and amputations also increases. All diabetics should know that even mild elevations in blood pressure can be detrimental to health. Studies have shown that diabetics with even a slight elevation in blood pressure have 2-3 times the risk of heart disease compared to individuals without diabetes.[93]
Blood pressure readings do vary but experts recommend that blood pressure should not range above 140/80. Secondly, high blood pressure is a silent disease and thus it is vital for all diabetics to regularly check their blood pressure or have it checked at a doctor's office on a regular basis. The American Diabetes Association recommends that all diabetics get their blood pressure measured by a health care professional at least 2-5 times a year.[94]
Treatment for diabetic patients with hypertension edit
Once blood pressure is found to be high in diabetics, there are ways to treat it:
Medications like the Angiotensin-converting enzyme inhibitors (ACEI) are widely used to control blood pressure in diabetics. These medications not only control blood pressure but also delay or prevent the development of kidney disease in diabetes. Many studies have shown that ACEI should be the drugs of first choice in diabetics with high blood pressure.[citation needed] Other medications used to treat high blood pressure include water pills. Sometimes, a combination of medications is used to treat high blood pressure. All diabetics should quit smoking. The combination of diabetes and smoking usually leads to amputations of the toes and feet. Measure your blood sugars regularly, and make sure that they are well balanced as the majority of complications of diabetes can be prevented by ensuring such blood sugars stay within normal limits.[95] It is also recommended to eat a healthy diet and avoid sugary foods and limit the intake of salt. Also, ensure that your cholesterol levels are under control. Exercise is a must for all diabetics. Walking twice a day for 30 minutes can be a fair substitute for those not engaged in intense gym activities. Losing weight is also beneficial as this has been shown to improve blood sugar control, increase insulin sensitivity and reduce blood pressure.[96]
References edit
- ^ a b c White WB (May 2009). "Defining the problem of treating the patient with hypertension and arthritis pain". The American Journal of Medicine. 122 (5 Suppl): S3–9. doi:10.1016/j.amjmed.2009.03.002. PMID 19393824.
- ^ O’Mahoney, P. R. A.; Wong, D. T.; Ray, J. G. (2008). "Retinal Vein Occlusion and Traditional Risk Factors for Atherosclerosis". JAMA Ophthalmology. 126 (5): 692–699. doi:10.1001/archopht.126.5.692. PMID 18474782.
- ^ Insull W (January 2009). "The pathology of atherosclerosis: plaque development and plaque responses to medical treatment". The American Journal of Medicine. 122 (1 Suppl): S3–S14. doi:10.1016/j.amjmed.2008.10.013. PMID 19110086.
- ^ Liapis CD, Avgerinos ED, Kadoglou NP, Kakisis JD (May 2009). "What a vascular surgeon should know and do about atherosclerotic risk factors". Journal of Vascular Surgery. 49 (5): 1348–54. doi:10.1016/j.jvs.2008.12.046. PMID 19394559.
- ^ Riccioni G (2009). "The effect of antihypertensive drugs on carotid intima media thickness: an up-to-date review". Current Medicinal Chemistry. 16 (8): 988–96. doi:10.2174/092986709787581923. PMID 19275607. Archived from the original on 2013-01-12. Retrieved 2009-06-20.
- ^ Safar ME, Jankowski P (February 2009). "Central blood pressure and hypertension: role in cardiovascular risk assessment". Clinical Science. 116 (4): 273–82. doi:10.1042/CS20080072. PMID 19138169.
- ^ Werner CM, Böhm M (June 2008). "The therapeutic role of RAS blockade in chronic heart failure". Therapeutic Advances in Cardiovascular Disease. 2 (3): 167–77. doi:10.1177/1753944708091777. PMID 19124420. S2CID 12972801.
- ^ Gaddam KK, Verma A, Thompson M, Amin R, Ventura H (May 2009). "Hypertension and cardiac failure in its various forms". The Medical Clinics of North America. 93 (3): 665–80. doi:10.1016/j.mcna.2009.02.005. PMID 19427498. Retrieved 2009-06-20.
- ^ Reisin E, Jack AV (May 2009). "Obesity and hypertension: mechanisms, cardio-renal consequences, and therapeutic approaches". The Medical Clinics of North America. 93 (3): 733–51. doi:10.1016/j.mcna.2009.02.010. PMID 19427502. Retrieved 2009-06-20.
- ^ a b c Agabiti-Rosei E (September 2008). "From macro- to microcirculation: benefits in hypertension and diabetes". Journal of Hypertension Supplement. 26 (3): S15–9. doi:10.1097/01.hjh.0000334602.71005.52. PMID 19363848.
- ^ Murphy BP, Stanton T, Dunn FG (May 2009). "Hypertension and myocardial ischemia". The Medical Clinics of North America. 93 (3): 681–95. doi:10.1016/j.mcna.2009.02.003. PMID 19427499. Retrieved 2009-06-20.
- ^ Tylicki L, Rutkowski B (February 2003). "[Hypertensive nephropathy: pathogenesis, diagnosis and treatment]". Polski Merkuriusz Lekarski (in Polish). 14 (80): 168–73. PMID 12728683.
- ^ Truong LD, Shen SS, Park MH, Krishnan B (February 2009). "Diagnosing nonneoplastic lesions in nephrectomy specimens". Archives of Pathology & Laboratory Medicine. 133 (2): 189–200. doi:10.5858/133.2.189. PMID 19195963. Archived from the original on 2020-03-28. Retrieved 2009-06-20.
- ^ Tracy RE, White S (February 2002). "A method for quantifying adrenocortical nodular hyperplasia at autopsy: some use of the method in illuminating hypertension and atherosclerosis". Annals of Diagnostic Pathology. 6 (1): 20–9. doi:10.1053/adpa.2002.30606. PMID 11842376.
- ^ Aronow WS (August 2008). "Hypertension and the older diabetic". Clinics in Geriatric Medicine. 24 (3): 489–501, vi–vii. doi:10.1016/j.cger.2008.03.001. PMID 18672184. Retrieved 2009-06-20.
- ^ Gardner AW, Afaq A (2008). "Management of Lower Extremity Peripheral Arterial Disease". Journal of Cardiopulmonary Rehabilitation and Prevention. 28 (6): 349–57. doi:10.1097/HCR.0b013e31818c3b96. PMC 2743684. PMID 19008688.
- ^ Novo S, Lunetta M, Evola S, Novo G (January 2009). "Role of ARBs in the blood hypertension therapy and prevention of cardiovascular events". Current Drug Targets. 10 (1): 20–5. doi:10.2174/138945009787122897. PMID 19149532. Archived from the original on 2013-01-12. Retrieved 2009-06-20.
- ^ a b c Steinmetz M, Nickenig G (April 2009). "[Cardiac sequelae of hypertension]". Der Internist (in German). 50 (4): 397–409. doi:10.1007/s00108-008-2289-3. PMID 19343394. S2CID 7660279.
- ^ a b c Hennersdorf MG, Strauer BE (March 2006). "[Hypertension and heart]". Medizinische Klinik (in German). 101 (Suppl 1): 27–30. PMID 16802514.
- ^ a b c Hennersdorf MG, Strauer BE (March 2007). "[The heart in hypertension]". Der Internist (in German). 48 (3): 236–45. doi:10.1007/s00108-006-1762-0. PMID 17260148. S2CID 22498249.
- ^ Motz W (October 2004). "[Right ventricle in arterial hypertension]". Der Internist (in German). 45 (10): 1108–16. doi:10.1007/s00108-004-1273-9. PMID 15351931. S2CID 25919141.
- ^ a b c Wachtell K, Devereux RB, Lyle PA, Okin PM, Gerdts E (December 2008). "The left atrium, atrial fibrillation, and the risk of stroke in hypertensive patients with left ventricular hypertrophy". Therapeutic Advances in Cardiovascular Disease. 2 (6): 507–13. doi:10.1177/1753944708093846. PMID 19124445. S2CID 9411507.
- ^ Petrović, Dejan; Stojimirović, Biljana (2008). "Hipertrofija leve komore kod bolesnlka koji se leče redovnim hemodijalizama" [Left ventricular hypertrophy in patients treated with regular hemodialyses]. Medicinski Pregled (in Serbian). 61 (7–8): 369–374. doi:10.2298/MPNS0808369P. PMID 19097374.
- ^ Cuspidi C, Sala C, Zanchetti A (December 2007). "Management of hypertension in patients with left ventricular hypertrophy". Current Hypertension Reports. 9 (6): 498–505. doi:10.1007/s11906-007-0091-6. PMID 18367014. S2CID 44337763.
- ^ Simko F (September 2007). "Statins: a perspective for left ventricular hypertrophy treatment". European Journal of Clinical Investigation. 37 (9): 681–91. doi:10.1111/j.1365-2362.2007.01837.x. PMID 17696957. S2CID 34378084.[dead link]
- ^ Wachtell K, Devereux RB, Lyle AP (August 2007). "The effect of angiotensin receptor blockers for preventing atrial fibrillation". Current Hypertension Reports. 9 (4): 278–83. doi:10.1007/s11906-007-0051-1. PMID 17686377. S2CID 24230854.
- ^ a b Herpin D (March 1999). "[Impact of arterial hypertension on the heart]". La Revue du praticien (in French). 49 (5): 491–4. PMID 10358398.
- ^ Parekh N, Maisel AS (March 2009). "Utility of B-natriuretic peptide in the evaluation of left ventricular diastolic function and diastolic heart failure". Current Opinion in Cardiology. 24 (2): 155–60. doi:10.1097/HCO.0b013e328320d82a. PMID 19532102.
- ^ Biria M, Howard PA, Vacek J (2008). "Do statins have a role in the management of diastolic dysfunction?". American Journal of Cardiovascular Drugs. 8 (5): 297–303. doi:10.2165/00129784-200808050-00002. PMID 18828641. S2CID 38191136.
- ^ Caserta MA, Milan A, Naso D, et al. (May 2007). "[Left ventricular diastolic function and dysfunction: a single cardiac target for various systemic diseases]". Giornale Italiano di Cardiologia (in Italian). 8 (5): 279–98. PMID 17650687.
- ^ Verma A, Solomon SD (May 2009). "Diastolic dysfunction as a link between hypertension and heart failure". The Medical Clinics of North America. 93 (3): 647–64. doi:10.1016/j.mcna.2009.02.013. PMID 19427497. Retrieved 2009-06-22.
- ^ Ellis CR, Di Salvo T (2007). "Myocarditis: basic and clinical aspects". Cardiology in Review. 15 (4): 170–7. doi:10.1097/CRD.0b013e31806450c4. PMID 17575480. S2CID 20513704.
- ^ Okoshi K, Guimarães JF, Di Muzio BP, Fernandes AA, Okoshi MP (March 2007). "[Diabetic cardiomyopathy]". Arquivos Brasileiros de Endocrinologia e Metabologia (in Portuguese). 51 (2): 160–7. doi:10.1590/s0004-27302007000200004. hdl:11449/11269. PMID 17505622.
- ^ a b Fukuta H, Little WC (May 2007). "Diagnosis of diastolic heart failure". Current Cardiology Reports. 9 (3): 224–8. doi:10.1007/BF02938354. PMID 17470335. S2CID 656249.
- ^ Schrader J (April 2009). "[Stroke and hypertension]". Der Internist (in German). 50 (4): 423–32. doi:10.1007/s00108-008-2291-9. PMID 19308341. S2CID 38815274.
- ^ Zeng C, Villar VA, Yu P, Zhou L, Jose PA (April 2009). "Reactive oxygen species and dopamine receptor function in essential hypertension". Clinical and Experimental Hypertension. 31 (2): 156–78. doi:10.1080/10641960802621283. PMC 3722595. PMID 19330604.
- ^ Varon J (October 2007). "Diagnosis and management of labile blood pressure during acute cerebrovascular accidents and other hypertensive crises". The American Journal of Emergency Medicine. 25 (8): 949–59. doi:10.1016/j.ajem.2007.02.032. PMID 17920983.
- ^ Sare GM, Geeganage C, Bath PM (2009). "High blood pressure in acute ischaemic stroke--broadening therapeutic horizons". Cerebrovascular Diseases. 27 (Suppl 1): 156–61. doi:10.1159/000200454. PMID 19342846. S2CID 5400230. Retrieved 2009-06-20.
- ^ Palm F, Urbanek C, Grau A (April 2009). "Infection, its treatment and the risk for stroke". Current Vascular Pharmacology. 7 (2): 146–52. doi:10.2174/157016109787455707. PMID 19355997. Archived from the original on 2013-04-14. Retrieved 2009-06-20.
- ^ Tanahashi N (April 2009). "[Roles of angiotensin II receptor blockers in stroke prevention]". Nippon Rinsho (in Japanese). 67 (4): 742–9. PMID 19348237.
- ^ a b c d e Loscalzo, Joseph; Fauci, Anthony S.; Braunwald, Eugene; Dennis L. Kasper; Hauser, Stephen L; Longo, Dan L. (2008). Harrison's principles of internal medicine. McGraw-Hill Medical. ISBN 978-0-07-147691-1.
- ^ Iadecola C, Park L, Capone C (March 2009). "Threats to the Mind: Aging, Amyloid, and Hypertension". Stroke. 40 (3 Suppl): S40–4. doi:10.1161/STROKEAHA.108.533638. PMC 2704500. PMID 19064785. Archived from the original on 2013-02-23. Retrieved 2009-06-22.
- ^ a b Erkinjuntti T, Gauthier S (2009). "The concept of vascular cognitive impairment". Dementia in Clinical Practice. Frontiers of Neurology and Neuroscience. Vol. 24. pp. 79–85. doi:10.1159/000197886. ISBN 978-3-8055-9015-0. PMID 19182465.
- ^ Birns J, Kalra L (February 2009). "Cognitive function and hypertension". Journal of Human Hypertension. 23 (2): 86–96. doi:10.1038/jhh.2008.80. PMID 18650838. S2CID 11574645.
- ^ a b Moretti R, Torre P, Antonello RM, Manganaro D, Vilotti C, Pizzolato G (2008). "Risk factors for vascular dementia: Hypotension as a key point". Vascular Health and Risk Management. 4 (2): 395–402. doi:10.2147/VHRM.S2434. PMC 2496988. PMID 18561514.
- ^ Solans-Laqué R, Bosch-Gil JA, Molina-Catenario CA, Ortega-Aznar A, Alvarez-Sabin J, Vilardell-Tarres M (November 2008). "Stroke and multi-infarct dementia as presenting symptoms of giant cell arteritis: report of 7 cases and review of the literature". Medicine. 87 (6): 335–44. doi:10.1097/MD.0b013e3181908e96. PMID 19011505.
- ^ Kuźma, Elżbieta; Lourida, Ilianna; Moore, Sarah F.; Levine, Deborah A.; Ukoumunne, Obioha C.; Llewellyn, David J. (August 2018). "Stroke and dementia risk: A systematic review and meta-analysis". Alzheimer's & Dementia. 14 (11): 1416–1426. doi:10.1016/j.jalz.2018.06.3061. hdl:2027.42/152961. ISSN 1552-5260. PMC 6231970. PMID 30177276.
- ^ Pantoni L, Poggesi A, Inzitari D (2009). "Cognitive decline and dementia related to cerebrovascular diseases: some evidence and concepts". Cerebrovascular Diseases. 27 (Suppl 1): 191–6. doi:10.1159/000200459. PMID 19342851. S2CID 3403376. Retrieved 2009-06-23.
- ^ Zekry D (2009). "Is it possible to treat vascular dementia?". Dementia in Clinical Practice. Frontiers of Neurology and Neuroscience. Vol. 24. pp. 95–106. doi:10.1159/000197888. ISBN 978-3-8055-9015-0. PMID 19182467.
- ^ Viswanathan A, Rocca WA, Tzourio C (January 2009). "Vascular risk factors and dementia: How to move forward?". Neurology. 72 (4): 368–74. doi:10.1212/01.wnl.0000341271.90478.8e. PMC 2677504. PMID 19171835.
- ^ Sorrentino G, Migliaccio R, Bonavita V (2008). "Treatment of vascular dementia: the route of prevention". European Neurology. 60 (5): 217–23. doi:10.1159/000151696. PMID 18756085. S2CID 6389257. Retrieved 2009-06-23.
- ^ Hall, John E.; Guyton, Arthur C. (2006). Textbook of medical physiology. St. Louis, Mo: Elsevier Saunders. p. 762. ISBN 978-0-7216-0240-0.
- ^ Müller-Wiefel DE (August 1988). "[The hypertensive crisis in childhood]". Wiener Klinische Wochenschrift (in German). 100 (16): 547–55. PMID 3055687.
- ^ Isles CG (February 1995). "Management of hypertensive crises". Scottish Medical Journal. 40 (1): 23–5. doi:10.1177/003693309504000110. PMID 7604239. S2CID 24448490.
- ^ Refai D, Botros JA, Strom RG, Derdeyn CP, Sharma A, Zipfel GJ (December 2008). "Spontaneous isolated convexity subarachnoid hemorrhage: presentation, radiological findings, differential diagnosis, and clinical course". Journal of Neurosurgery. 109 (6): 1034–41. doi:10.3171/JNS.2008.109.12.1034. PMID 19035716.
- ^ O'Hara McCoy H (February 2008). "Posterior reversible encephalopathy syndrome: an emerging clinical entity in adult, pediatric, and obstetric critical care". Journal of the American Academy of Nurse Practitioners. 20 (2): 100–6. doi:10.1111/j.1745-7599.2007.00292.x. PMID 18271765. S2CID 208287631.[dead link]
- ^ Walsh JB (October 1982). "Hypertensive retinopathy. Description, classification, and prognosis". Ophthalmology. 89 (10): 1127–31. doi:10.1016/s0161-6420(82)34664-3. PMID 7155523.
- ^ Liebreich R. Ophthalmoskopischer Befund bei Morbus Brightii. Albrecht von Graefes Arch Ophthalmol 1859; 5: 265–268.
- ^ a b c Tso MO, Jampol LM (October 1982). "Pathophysiology of hypertensive retinopathy". Ophthalmology. 89 (10): 1132–45. doi:10.1016/s0161-6420(82)34663-1. PMID 7155524.
- ^ Wong TY, Mitchell P (November 2004). "Hypertensive retinopathy". The New England Journal of Medicine. 351 (22): 2310–7. doi:10.1056/NEJMra032865. PMID 15564546.
- ^ Pache M, Kube T, Wolf S, Kutschbach P (June 2002). "Do angiographic data support a detailed classification of hypertensive fundus changes?". Journal of Human Hypertension. 16 (6): 405–10. doi:10.1038/sj.jhh.1001402. PMID 12037695. S2CID 28083513.
- ^ Krzesinski JM, Cohen EP (2007). "Hypertension and the kidney". Acta Clinica Belgica. 62 (1): 5–14. doi:10.1179/acb.2007.002. PMID 17451140. S2CID 40916501.
- ^ Monhart V (May 2008). "[Diabetes mellitus, hypertension and kidney]". Vnitr̆ní Lékar̆ství (in Czech). 54 (5): 499–504, 507. PMID 18630636.
- ^ Hohenstein K, Watschinger B (2008). "[Hypertension and the kidney]". Wiener Medizinische Wochenschrift (in German). 158 (13–14): 359–64. doi:10.1007/s10354-008-0558-3. PMID 18677585. S2CID 195686488.
- ^ Khosla N, Kalaitzidis R, Bakris GL (May 2009). "The kidney, hypertension, and remaining challenges". The Medical Clinics of North America. 93 (3): 697–715, Table of Contents. doi:10.1016/j.mcna.2009.02.001. PMID 19427500. Retrieved 2009-06-23.
- ^ Ponnuchamy B, Khalil RA (April 2009). "Cellular mediators of renal vascular dysfunction in hypertension". American Journal of Physiology. 296 (4): R1001–18. doi:10.1152/ajpregu.90960.2008. PMC 2698613. PMID 19225145.
- ^ Niang A (2008). "[Arterial hypertension and the kidney]". Dakar Médical (in French). 53 (1): 1–6. PMID 19102111.
- ^ Palmer BF (October 2008). "Hypertension management in patients with chronic kidney disease". Current Hypertension Reports. 10 (5): 367–73. doi:10.1007/s11906-008-0069-z. PMID 18775113. S2CID 24933057.
- ^ a b Marín R, Gorostidi M, Fernández-Vega F, Alvarez-Navascués R (December 2005). "Systemic and glomerular hypertension and progression of chronic renal disease: the dilemma of nephrosclerosis". Kidney International Supplements. 68 (99): S52–6. doi:10.1111/j.1523-1755.2005.09910.x. PMID 16336577.
- ^ Schmitz A (September 1997). "Microalbuminuria, blood pressure, metabolic control, and renal involvement: longitudinal studies in white non-insulin-dependent diabetic patients". American Journal of Hypertension. 10 (9 Pt 2): 189S–197S. doi:10.1016/S0895-7061(97)00152-0. PMID 9324121.
- ^ Lindhorst J, Alexander N, Blignaut J, Rayner B (2007). "Differences in hypertension between blacks and whites: an overview". Cardiovascular Journal of Africa. 18 (4): 241–7. PMC 4170224. PMID 17940670.
- ^ Swift PA, Macgregor GA (January 2004). "Genetic variation in the epithelial sodium channel: a risk factor for hypertension in people of African origin". Advances in Renal Replacement Therapy. 11 (1): 76–86. doi:10.1053/j.arrt.2003.10.011. PMID 14730541.
- ^ Ergul A (July 2000). "Hypertension in black patients: an emerging role of the endothelin system in salt-sensitive hypertension". Hypertension. 36 (1): 62–7. doi:10.1161/01.hyp.36.1.62. PMID 10904013.
- ^ Ferrari P, Krozowski Z (April 2000). "Role of the 11beta-hydroxysteroid dehydrogenase type 2 in blood pressure regulation". Kidney International. 57 (4): 1374–81. doi:10.1046/j.1523-1755.2000.00978.x. PMID 10760070.
- ^ Campese VM (May 1996). "The kidney in the hypertensive black". Ethnicity & Health. 1 (2): 145–51. doi:10.1080/13557858.1996.9961781. PMID 9395558.
- ^ Bidani AK, Griffin KA (January 2002). "Long-term renal consequences of hypertension for normal and diseased kidneys". Current Opinion in Nephrology and Hypertension. 11 (1): 73–80. doi:10.1097/00041552-200201000-00011. PMID 11753090. S2CID 23305725.
- ^ Johnson RJ, Rodriguez-Iturbe B, Kang DH, Feig DI, Herrera-Acosta J (March 2005). "A unifying pathway for essential hypertension". American Journal of Hypertension. 18 (3): 431–40. doi:10.1016/j.amjhyper.2004.08.035. PMID 15797666.
- ^ Kwoh C, Shannon MB, Miner JH, Shaw A (2006). "Pathogenesis of nonimmune glomerulopathies". Annual Review of Pathology. 1: 349–74. doi:10.1146/annurev.pathol.1.110304.100119. PMID 18039119.
- ^ Stoian M, Radulian G, Chiţac D, Simion E, Stoica V (2007). "A clinical approach in regression of glomerulosclerosis". Romanian Journal of Internal Medicine. 45 (2): 215–8. PMID 18333378.
- ^ Ono H, Ono Y (November 1997). "Nephrosclerosis and hypertension". The Medical Clinics of North America. 81 (6): 1273–88. doi:10.1016/S0025-7125(05)70582-4. PMID 9356598.
- ^ Muirhead EE, Pitcock JA (December 1989). "Histopathology of severe renal vascular damage in blacks". Clinical Cardiology. 12 (Suppl 4): IV58–65. doi:10.1002/clc.4960121312. PMID 2620472. S2CID 41855935.
- ^ a b Dustan HP, Curtis JJ, Luke RG, Rostand SG (December 1987). "Systemic hypertension and the kidney in black patients". The American Journal of Cardiology. 60 (17): 73I–77I. doi:10.1016/0002-9149(87)90464-4. PMID 3687809.
- ^ Schwartz GL, Strong CG (September 1987). "Renal parenchymal involvement in essential hypertension". The Medical Clinics of North America. 71 (5): 843–58. doi:10.1016/S0025-7125(16)30812-4. PMID 3306206.
- ^ Cimprich RE, Ziemba LJ, Kutz SA, Robertson JL, Cockrell B (1986). "Experimentally induced malignant hypertension in beagle dogs". Toxicologic Pathology. 14 (2): 183–7. doi:10.1177/019262338601400206. PMID 3764316. S2CID 25800184.
- ^ Queiroz FP, Rojo-Ortega JM, Genest J (1980). "Metaischemic (post-Goldblatt) hypertensive vascular disease in rats". Hypertension. 2 (6): 765–70. doi:10.1161/01.hyp.2.6.765. PMID 7461792. S2CID 1587443.
- ^ Weller RO (May 1979). "Vascular pathology in hypertension". Age and Ageing. 8 (2): 99–103. doi:10.1093/ageing/8.2.99. PMID 463685.
- ^ Sinclair RA, Antonovych TT, Mostofi FK (September 1976). "Renal proliferative arteriopathies and associated glomerular changes: a light and electron microscopic study". Human Pathology. 7 (5): 565–88. doi:10.1016/S0046-8177(76)80103-7. PMID 987010.
- ^ Linz W, Becker RH, Schölkens BA, Wiemer G, Keil M, Langer KH (December 1998). "Nephroprotection by long-term ACE inhibition with ramipril in spontaneously hypertensive stroke prone rats". Kidney International. 54 (6): 2037–44. doi:10.1046/j.1523-1755.1998.00208.x. PMID 9853269.
- ^ Diabetes and Hypertension Archived 2009-04-17 at the Wayback Machine Medical Journal of Australia. 2010-02-09
- ^ Chiriaco M, et al. (2019). "Association between blood pressure variability, cardiovascular disease and mortality in type 2 diabetes: A systematic review and meta‐analysis". Diabetes, Obesity and Metabolism. 21 (12): 2587–2598. doi:10.1111/dom.13828. PMID 31282073. S2CID 195829708.
- ^ Nuyujukian DS, Koska J, Bahn G, Reaven PD, Zhou JJ (July 2020). "Blood Pressure Variability and Risk of Heart Failure in ACCORD and the VADT". Diabetes Care. 43 (7): 1471–1478. doi:10.2337/dc19-2540. hdl:10150/641980. PMC 7305004. PMID 32327422.
- ^ Nuyujukian DS, Zhou JJ, Koska J, Reaven PD (2021). "Refining determinants of associations of visit-to-visit blood pressure variability with cardiovascular risk: results from the Action to Control Cardiovascular Risk in Diabetes Trial". Journal of Hypertension. 39 (11): 2173–2182. doi:10.1097/hjh.0000000000002931. PMC 8500916. PMID 34232160.
- ^ Diabetes associated to Hypertension Archived 2015-09-07 at the Wayback Machine About health portal. 2010-02-09
- ^ Medical Journal of Australia. "Hypertension and Diabetes overview" Archived 2009-04-17 at the Wayback Machine 2010-02-09.
- ^ Diabetes Hypertension Guidelines: Treatment And Symptoms Archived 2010-02-09 at the Wayback Machine 2010-02-09
- ^ American Academy of Family Physicians. "Controlling Hypertension in Patients with Diabetes" 2010-02-09.


