
Summary
Enoxaparin sodium, sold under the brand name Lovenox among others, is an anticoagulant medication (blood thinner).[11] It is used to treat and prevent deep vein thrombosis (DVT) and pulmonary embolism (PE) including during pregnancy and following certain types of surgery.[11] It is also used in those with acute coronary syndrome (ACS) and heart attacks.[11] It is given by injection just under the skin or into a vein.[11] It is also used during hemodialysis.[8][10]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Lovenox, Clexane, Xaparin, others |
| Biosimilars | Arovi, Axberi,[1] Axberi HP,[1] Exarane,[2] Exarane Forte,[2] Enoxapo,[3] Inclunox, Inclunox HP, Inhixa, Noromby, Noromby HP, Redesca, Redesca HP, Thorinane |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a696006 |
| License data |
|
| Pregnancy category | |
| Routes of administration | Subcutaneous , intravenous |
| ATC code |
|
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Elimination half-life | 4.5 hours |
| Identifiers | |
| CAS Number |
|
| PubChem CID |
|
| IUPHAR/BPS |
|
| DrugBank |
|
| ChemSpider |
|
| UNII |
|
| KEGG |
|
| ChEMBL |
|
| CompTox Dashboard (EPA) |
|
| ECHA InfoCard | 100.029.698 |
| Chemical and physical data | |
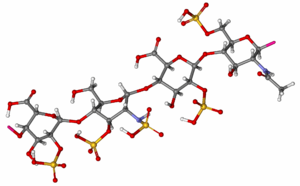
| Formula | (C26H40N2O36S5)n |
| Molar mass | 4500 g/mol (average) |
| | |
Common side effects include bleeding, fever, and swelling of the legs.[11] Bleeding may be serious especially in those who are undergoing a spinal tap.[11] Use during pregnancy appears to be safe for the baby.[11] Enoxaparin is in the low molecular weight heparin family of medications.[11]
Enoxaparin was first made in 1981 and approved for medical use in 1993.[12][11] It is on the World Health Organization's List of Essential Medicines.[13] Enoxaparin is sold under several brand names and is available as a generic medication.[11] Enoxaparin is made from heparin.[12] In 2020, it was the 350th most commonly prescribed medication in the United States, with more than 500 thousand prescriptions.[14]
Medical uses edit
- Treatment of unstable angina (UA) and non-ST elevated myocardial infarction (NSTEMI), administered concurrently with aspirin
- DVT and pulmonary embolism prophylaxis in bed-ridden patients
- DVT prophylaxis in knee replacement surgery
- DVT prophylaxis in hip replacement surgery
- DVT prophylaxis in abdominal surgery
- Treatment of DVT with or without pulmonary embolism
- Treatment of DVT inpatient, with ST-segment elevation myocardial infarction (STEMI)[9]
- Bridging treatment for those with INR below therapeutic range
Monitoring edit
Enoxaparin has predictable absorption, bioavailability, and distribution therefore monitoring is not typically done. However, there are instances where monitoring may be beneficial for special populations, for example individuals with kidney insufficiency or those that are obese. In this case, anti-Xa units can be measured and dosing adjusted accordingly.[9]
Reversal agent edit
Protamine sulfate is less effective at reversing enoxaparin compared to heparin, with a maximum neutralization of approximately 60% of the anti-factor Xa effect.[9]
Pregnancy edit
- Enoxaparin is a FDA pregnancy category B drug which means enoxaparin is not expected to cause harm to an unborn baby when used during pregnancy.[9]
- Enoxaparin does not cross the placenta therefore it is unlikely an unborn baby would be exposed to it.[9]
- Some fetal deaths have been reported by women who used enoxaparin during pregnancy, but it is unclear if enoxaparin caused these deaths.[9]
- The multiple-dose vials of the brand name enoxaparin (Lovenox) contain 15 mg benzyl alcohol per 1 mL as a preservative. Premature infants who have been given large amounts of benzyl alcohol (99–405 mg/kg/day) have experienced "gasping syndrome".[9][15]
- Although enoxaparin is used to prevent blood clots, pregnancy alone can raise a woman's risk of clotting.[9]
Side effects edit
Uncommon (<1%)
- In people with unstable angina or non-Q-wave myocardial infarction:
- Atrial fibrillation, heart failure, lung edema, pneumonia: ≥ 0.5%v
Common (>1%)
- Thrombocytopenia, i.e. can be associated with heparin-induced thrombocytopenia (0.5-5.0% of persons treated for at least five days)[16]
- Elevations in serum aminotransferases: 5.9%-6.1%[9]
- In people undergoing abdominal or colorectal surgery:
- Bleeding, anemia, ecchymosis: ≥ 2%[9]
- In persons undergoing hip or knee replacement:
- In persons with severely restricted mobility during acute illness:
- In people being treated for deep vein thrombosis:
Frequency under investigation
- Local reactions: local irritation, pain, hematoma, ecchymosis, erythema[9]
- Bleeding[9]
- Hyperkalemia[9]
- Transaminitis[9]
- Hemorrhage[9]
Boxed warning edit
The FDA issued a revision to the boxed warning for enoxaparin in October 2013.[17] The revision recommends exercising caution regarding when spinal catheters are placed and removed in persons taking enoxaparin for spinal puncture or neuroaxial anesthesia.[18] It may be necessary to delay anticoagulant dosing in these persons in order to decrease the risk for spinal or epidural hematomas, which can manifest as permanent or long-term paralysis.[18] Persons at risk for hematomas may present with indwelling epidural catheters, concurrent use of medications that worsen bleeding states such as non-steroidal anti-inflammatory drugs (NSAIDs), or a past medical history of epidural or spinal punctures, spinal injury, or spinal deformations.[17] The FDA recommends that at-risk persons be monitored for bleeding and neurological changes.[17][19]
Pharmacology edit
Mechanism of action edit
Enoxaparin binds to and potentiates antithrombin (a circulating anticoagulant) to form a complex that irreversibly inactivates clotting factor Xa.[20] It has less activity against factor IIa (thrombin) compared to unfractionated heparin (UFH) due to its low molecular weight.[21]
Pharmacokinetics edit
Absorption: Bioavailability (subcutaneous injection) ~ 100%[17]
Distribution: Volume of distribution (anti-Factor Xa activity) = 4.3 liters[17]
Metabolism: Enoxaparin is metabolized in the liver into low molecular weight species by either or both desulfation and depolymerization.[17]
Elimination: A single dose of a subcutaneous injection of enoxaparin has an elimination half-life of 4.5 hours.[17] Approximately 10–40% of the active and inactive fragments from a single dose are excreted by the kidneys.[17] Dose adjustments based on kidney function are necessary in persons with reduced kidney function.[17]
Drug class edit
Enoxaparin belongs to the class of drugs known as low molecular weight heparins. Other drugs in this class include dalteparin, fondaparinux and tinzaparin.[22]
Biosimilars edit
In September 2016, Inhixa and Thorinane were approved for use in the European Union.[10][23] Thorinane was withdrawn from the market in October 2019.[24]
In March 2017, Enoxaparin BECAT, Laboratorios ROVI (Spain) obtained marketing authorization in twenty six countries in Europe. The product is now available in Europe.[25]
In October 2020, Noromby and Noromby HP, were approved for medical use in Canada.[26]
In November 2020, Inclunox and Inclunox HP were approved for medical use in Canada.[27]
In December 2020, Redesca and Redesca HP were approved for medical use in Canada.[28]
References edit
- ^ a b "Summary Basis of Decision (SBD) for Axberi/Axberi HP". Health Canada. 26 January 2024. Archived from the original on 24 February 2024. Retrieved 24 February 2024.
- ^ a b c d https://www.tga.gov.au/resources/auspmd/exaraneexarane-forte Archived 2 January 2024 at the Wayback Machine [bare URL]
- ^ a b c "Enoxapo Australian prescription medicine decision summary". Therapeutic Goods Administration (TGA). 28 February 2020. Archived from the original on 26 February 2020. Retrieved 17 August 2020.
- ^ "Enoxaparin Use During Pregnancy". Drugs.com. 15 July 2019. Archived from the original on 27 October 2020. Retrieved 16 August 2020.
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ "AusPAR: Exarane/Exarane Forte". Therapeutic Goods Administration (TGA). 4 March 2024. Retrieved 31 March 2024.
- ^ "Summary Basis of Decision - Elonox/Elonox HP". Health Canada. 28 March 2023. Archived from the original on 25 April 2023. Retrieved 24 April 2023.
- ^ a b "Clexane Forte Syringes - Summary of Product Characteristics (SmPC)". emc. Archived from the original on 26 September 2018. Retrieved 12 October 2020.
- ^ a b c d e f g h i j k l m n o p q r s "Lovenox- enoxaparin sodium injection". DailyMed. U.S. National Library of Medicine. 28 April 2020. Archived from the original on 4 August 2020. Retrieved 16 August 2020.
- ^ a b c "Inhixa EPAR". European Medicines Agency (EMA). 17 September 2018. Archived from the original on 29 October 2020. Retrieved 2 April 2020.
- ^ a b c d e f g h i j "Enoxaparin Sodium". The American Society of Health-System Pharmacists. Archived from the original on 21 December 2016. Retrieved 8 December 2016.
- ^ a b Northern Neonatal Network (2008). "Enoxaparin". Neonatal Formulary: Drug Use in Pregnancy and the First Year of Life. John Wiley & Sons. p. 96. ISBN 9780470750353. Archived from the original on 20 December 2016.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ "Enoxaparin - Drug Usage Statistics". ClinCalc. Archived from the original on 7 November 2022. Retrieved 7 October 2022.
- ^ Gershanik J, Boecler B, Ensley H, McCloskey S, George W (November 1982). "The gasping syndrome and benzyl alcohol poisoning". The New England Journal of Medicine. 307 (22): 1384–1388. doi:10.1056/NEJM198211253072206. PMID 7133084.
- ^ Levy JH, Tanaka KA, Hursting MJ (September 2007). "Reducing thrombotic complications in the perioperative setting: an update on heparin-induced thrombocytopenia". Anesthesia and Analgesia. 105 (3): 570–582. doi:10.1213/01.ane.0000277497.70701.47. PMID 17717208. S2CID 25103749.
- ^ a b c d e f g h i "ENOXAPARIN SODIUM- enoxaparin sodium injection". DailyMed. U.S. National Library of Medicine. Archived from the original on 19 October 2015. Retrieved 5 November 2015.
- ^ a b "Drug Safety and Availability - FDA Drug Safety Communication: Updated recommendations to decrease risk of spinal column bleeding and paralysis in patients on low molecular weight heparins". Center for Drug Evaluation and Research. U.S. Food and Drug Administration. Archived from the original on 30 October 2015. Retrieved 5 November 2015.
- ^ Office of the Commissioner. "Safety Information - Lovenox (enoxaparin sodium) injection". U.S. Food and Drug Administration. Archived from the original on 4 March 2016. Retrieved 5 November 2015.
- ^ Alldredge BK, Corelli RL, Ernst ME, Guglielmo BJ, Jacobson PA, Kradjan WA, Williams BR (February 2012). Koda-Kimble and Young's Applied Therapeutics: The Clinical Use of Drugs (Tenth ed.). Lippincott Williams & Wilkins. pp. 347–348. ISBN 978-1-60913-713-7.
- ^ Trevor AJ, Katzung BG, Masters SB (2012). Basic & Clinical Pharmacology. McGraw-Hill Medical. ISBN 978-0-07-176401-8.
- ^ "LowMolecularWeightHeparins". livertox.nih.gov. 2012. PMID 31643176. Archived from the original on 28 August 2015. Retrieved 5 November 2015.
- ^ "Thorinane EPAR". European Medicines Agency (EMA). 17 September 2018. Archived from the original on 30 December 2019. Retrieved 2 April 2020.
- ^ "Public statement on Thorinane: Cessation of validity of the marketing authorisation in the European Union" (PDF). Archived (PDF) from the original on 28 August 2021. Retrieved 2 April 2020.
- ^ "To The National Stock Market Commission" (PDF). Archived (PDF) from the original on 28 August 2021. Retrieved 29 May 2020.
- ^ "Summary Basis of Decision (SBD) for Noromby/Noromby HP". Health Canada. 23 October 2014. Archived from the original on 30 May 2022. Retrieved 29 May 2022.
- ^ "Summary Basis of Decision (SBD) for Inclunox/Inclunox HP". Health Canada. 23 October 2014. Archived from the original on 30 May 2022. Retrieved 29 May 2022.
- ^ "Summary Basis of Decision (SBD) for Redesca/Redesca HP". Health Canada. 23 October 2014. Archived from the original on 30 May 2022. Retrieved 29 May 2022.


