
Summary
Microscopic colitis refers to two related medical conditions which cause diarrhea: collagenous colitis and lymphocytic colitis.[2][3] Both conditions are characterized by the presence of chronic non-bloody watery diarrhea, normal appearances on colonoscopy and characteristic histopathology findings of inflammatory cells.[1]
| Microscopic colitis | |
|---|---|
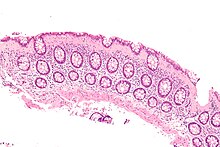 | |
| Micrograph of collagenous colitis, a type of microscopic colitis. H&E stain. | |
| Specialty | Gastroenterology |
| Symptoms | Persistent diarrhea |
| Types | Lymphocytic colitis, collagenous colitis |
| Diagnostic method | Endoscopic biopsy of colonic mucosa |
| Differential diagnosis | Bile acid diarrhea, celiac disease, lactose malabsorption, Crohn's disease, ulcerative colitis, infectious colitis[1][2] |
| Medication | Loperamide, Bismuth subsalicylate, Budesonide |
| Frequency | 103 cases per 100,000 persons[2] |
Signs and symptoms edit
The main symptom is persistent non-bloody watery diarrhea, which may be profuse. People may also experience abdominal pain, fecal incontinence, and unintentional weight loss.[1] Microscopic colitis is the diagnosis in around 10% of cases investigated for chronic non-bloody diarrhea.[2]
Associated conditions edit
A higher incidence of autoimmune diseases, for example arthritis, Sjögren's syndrome, thyroid disorders, and celiac disease, has been reported in people with microscopic colitis.[1] Associations with various drugs have been found, especially proton pump inhibitors, H2 blockers, selective serotonin reuptake inhibitors (SSRIs), and non-steroidal anti-inflammatory drugs (NSAIDs).[1][2] Bile acid diarrhea is found in 41% of patients with collagenous colitis and 29% with lymphocytic colitis.[3] Additionally, cigarette smoking has been identified as a significant risk factor of microscopic colitis.[1]
Diagnosis edit
Colonoscopic appearances are normal or near normal. As the changes are often patchy, an examination limited to the rectum may miss cases of microscopic colitis, and so a full colonoscopy is necessary.[2] Multiple colonic biopsies are taken in order to make the diagnosis.[1] Histological features of colonic biopsies indicating microscopic colitis are: greater than 20 intraepithelial lymphocytes per 100 epithelial cells and, additionally, 10-20 μm of a thickened subepithelial collagen band in collagenous colitis.[1] Inflammation of the lamina propria, with mainly mononuclear cells, may be observed in collagenous colitis.[1]
Pathology edit
Microscopic colitis is characterized by an increase in inflammatory cells, particularly lymphocytes, in colonic biopsies with an otherwise normal appearance and architecture of the colon.[2] Inflammatory cells are increased both in the surface epithelium ("intraepithelial lymphocytes") and in the lamina propria. The key feature is more than 20 intra-epithelial lymphocytes per 100 epithelial cells.[2] These are the principal features of lymphocytic colitis. An additional distinguishing feature of collagenous colitis is a thickened subepithelial collagen layer, which may be up to 30 micrometres thick, that occurs in addition to the features found in lymphocytic colitis.[1] The fact that the two types of microscopic colitis share many features including epidemiology, risk factors and, response to therapy has led to the suggestion that they are actually subtypes of the same disease.[3]
Differential diagnosis edit
Differential diagnoses, which should be ruled out, include bile acid diarrhea, lactose malabsorption, celiac disease, Crohn's disease, ulcerative colitis, and infectious colitis.[1][2]
Treatment edit
Lymphocytic and collagenous colitis have both been shown in randomized, placebo-controlled trials to respond well to budesonide, a glucocorticoid.[4][5] Budesonide formulated to be active in the distal colon and rectum is effective for both active disease and in the prevention of relapse.[2][6] However, relapse occurs frequently after withdrawal of therapy.[1]
Studies of a number of other agents including antidiarrheals, bismuth subsalicylate (Pepto-Bismol), mesalazine/mesalamine (alone or in combination with cholestyramine), systemic corticosteroids, cholestyramine, immunomodulators, and probiotics have shown to be less effective than budesonide for treating both forms of microscopic colitis.[1][2][7][8]
Anti-TNF inhibitors. split ileostomy, diverting ileostomy, and subtotal colectomy are options for management of steroid-dependent or refractory microscopic colitis.[1][9] Currently, the need to resort to surgery is limited considering the improvement of drug therapy options.[9] However, surgery is still considered for patients with severe, unresponsive microscopic colitis.[9]
Prognosis edit
The prognosis for lymphocytic colitis and collagenous colitis is good, and both conditions are considered to be benign.[10] The majority of people afflicted with the conditions recover from their diarrhea, and their histological abnormalities resolve,[5] although relapses commonly occur if maintenance treatment is not continued.[1][2]
Epidemiology edit
Incidence and prevalence of microscopic colitis nears those of ulcerative colitis and Crohn's disease.[11] Studies in North America found incidence rates of 7.1 per 100,000 person-years and 12.6 per 100,000 person-years for collagenous colitis for lymphocytic colitis, respectively.[11] Prevalence has been estimated as 103 cases per 100,000 persons.[2]
People who develop microscopic colitis are characteristically, though not exclusively, middle-aged females. The average age of diagnosis is 65 but 25% of cases are diagnosed below the age of 45.[2]
History edit
The condition of microscopic colitis was first described as such in 1982.[12] Lymphocytic colitis was described in 1989.[13] Collagenous colitis was recognised earlier, in 1976.[14]
References edit
- ^ a b c d e f g h i j k l m n o Park, Tina; Cave, David; Marshall, Christopher (2015-08-07). "Microscopic colitis: A review of etiology, treatment and refractory disease". World Journal of Gastroenterology. 21 (29): 8804–8810. doi:10.3748/wjg.v21.i29.8804. ISSN 1007-9327. PMC 4528022. PMID 26269669.
- ^ a b c d e f g h i j k l m n Münch A, Aust D, Bohr J, Bonderup O, Fernández Bañares F, Hjortswang H, et al. (2012). "Microscopic colitis: Current status, present and future challenges: statements of the European Microscopic Colitis Group". J Crohns Colitis. 6 (9): 932–45. doi:10.1016/j.crohns.2012.05.014. PMID 22704658.
- ^ a b c Rasmussen MA, Munck LK (2012). "Systematic review: are lymphocytic colitis and collagenous colitis two subtypes of the same disease - microscopic colitis?". Aliment Pharmacol Ther. 36 (2): 79–90. doi:10.1111/j.1365-2036.2012.05166.x. PMID 22670660.
- ^ Chande, N; Al Yatama, N; Bhanji, T; Nguyen, TM; McDonald, JW; MacDonald, JK (13 July 2017). "Interventions for treating lymphocytic colitis". Cochrane Database of Systematic Reviews. 7 (11): CD006096. doi:10.1002/14651858.CD006096.pub4. PMC 6483541. PMID 28702956.
- ^ a b Fernández-Bañares F, Salas A, Esteve M, Espinós J, Forné M, Viver J (2003). "Collagenous and lymphocytic colitis. evaluation of clinical and histological features, response to treatment, and long-term follow-up". Am J Gastroenterol. 98 (2): 340–7. doi:10.1111/j.1572-0241.2003.07225.x. PMID 12591052. S2CID 1983209.
- ^ O'Donnell, Sarah; O'Morain, Colm A. (2016-10-19). "Therapeutic benefits of budesonide in gastroenterology". Therapeutic Advances in Chronic Disease. 1 (4): 177–186. doi:10.1177/2040622310379293. ISSN 2040-6223. PMC 3513866. PMID 23251737.
- ^ Chande, Nilesh; Al Yatama, Noor; Bhanji, Tania; Nguyen, Tran M.; McDonald, John Wd; MacDonald, John K. (13 July 2017). "Interventions for treating lymphocytic colitis". The Cochrane Database of Systematic Reviews. 7 (11): CD006096. doi:10.1002/14651858.CD006096.pub4. ISSN 1469-493X. PMC 6483541. PMID 28702956.
- ^ Kafil, Tahir S.; Nguyen, Tran M.; Patton, Petrease H.; MacDonald, John K.; Chande, Nilesh; McDonald, John Wd (11 November 2017). "Interventions for treating collagenous colitis". The Cochrane Database of Systematic Reviews. 2017 (11): CD003575. doi:10.1002/14651858.CD003575.pub6. ISSN 1469-493X. PMC 6486307. PMID 29127772.
- ^ a b c Bohr, Johan; Wickbom, Anna; Hegedus, Agnes; Nyhlin, Nils; Hultgren Hörnquist, Elisabeth; Tysk, Curt (2014-08-21). "Diagnosis and management of microscopic colitis: current perspectives". Clinical and Experimental Gastroenterology. 7: 273–284. doi:10.2147/CEG.S63905. ISSN 1178-7023. PMC 4144984. PMID 25170275.
- ^ Mullhaupt B, Güller U, Anabitarte M, Güller R, Fried M (1998). "Lymphocytic colitis: clinical presentation and long term course". Gut. 43 (5): 629–33. doi:10.1136/gut.43.5.629. PMC 1727313. PMID 9824342.
- ^ a b Storr, Martin Alexander (2013-04-18). "Microscopic Colitis: Epidemiology, Pathophysiology, Diagnosis and Current Management—An Update 2013". ISRN Gastroenterology. 2013: 352718. doi:10.1155/2013/352718. ISSN 2090-4398. PMC 3654232. PMID 23691336.
- ^ Kingham JG, Levison DA, Ball JA, Dawson AM (1982). "Microscopic colitis-a cause of chronic watery diarrhoea". Br Med J (Clin Res Ed). 285 (6355): 1601–4. doi:10.1136/bmj.285.6355.1601. PMC 1500804. PMID 6128051.
- ^ Lazenby AJ, Yardley JH, Giardiello FM, Jessurun J, Bayless TM (1989). "Lymphocytic ("microscopic") colitis: a comparative histopathologic study with particular reference to collagenous colitis". Hum. Pathol. 20 (1): 18–28. doi:10.1016/0046-8177(89)90198-6. PMID 2912870.
- ^ Bogomoletz WV, Adnet JJ, Birembaut P, Feydy P, Dupont P (1980). "Collagenous colitis: an unrecognised entity". Gut. 21 (2): 164–8. doi:10.1136/gut.21.2.164. PMC 1419351. PMID 7380341.
External links edit
- MayoClinic.com


