Summary
Prostatic acid phosphatase (PAP), also prostatic specific acid phosphatase (PSAP), is an enzyme produced by the prostate. It may be found in increased amounts in men who have prostate cancer or other diseases.
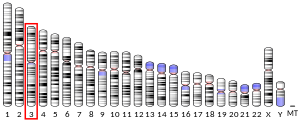
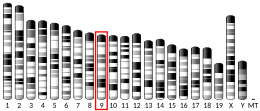
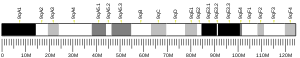
| ACP3 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | ACP3, 5'-NT, TM-PAP, ACP-3, acid phosphatase 3, acid phosphatase, prostate, ACPP | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 171790 MGI: 1928480 HomoloGene: 55552 GeneCards: ACP3 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| EC number | 3.1.3.5 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
The highest levels of acid phosphatase are found in metastasized prostate cancer. Diseases of the bone, such as Paget's disease or hyperparathyroidism, diseases of blood cells, such as sickle-cell disease or multiple myeloma or lysosomal storage diseases, such as Gaucher's disease, will show moderately increased levels.
Certain medications can cause temporary increases or decreases in acid phosphatase levels. Manipulation of the prostate gland through massage, biopsy or rectal exam before a test may increase the level.
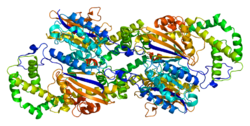
Its physiological function may be associated with the liquefaction process of semen.[5]
Use in prostatic cancer prognosis edit
Serum marker edit
PAP was used to monitor and assess progression of prostate cancer until the introduction of prostate specific antigen (PSA), which has now largely displaced it. Subsequent work, suggested that it has a role in prognosticating intermediate and high-risk prostate cancer, and led to renewed interest in it as a biomarker.[6]
Immunohistochemistry edit
PAP immunohistochemical staining is often used with PSA (staining), by pathologists, to help distinguish poorly differentiated carcinomas. For example, poorly differentiated prostate adenocarcinoma (prostate cancer) and urothelial carcinoma (bladder cancer) may appear similar under the microscope, but PAP and PSA staining can help differentiate them;[7] prostate adenocarcinoma often stains with PSA and/or PAP, while urothelial carcinoma does not.[citation needed]
HIV edit
PAP may play an important role in the transmission of HIV. Researchers at the University of Ulm in Germany found that PAP forms fibers made of amyloid. They called the fibers semen-derived enhancer of virus infection (SEVI) and showed that they capture HIV virions promoting their attachment to target cells. The association of PAP with HIV may increase the ability of the virus to infect human cells "by several orders of magnitude." PAP may be a future target of efforts to combat the spread of HIV infection.[8]
Pain suppression edit
A study at the University of North Carolina and University of Helsinki suggested that PAP could have potent antinociceptive, antihyperalgesic, and antiallodynic effects that last longer than morphine. One dose of PAP lasted for up to three days, much longer than the five hours gained with a single dose of morphine. When in distress, nerve cells release a chemical known as adenosine triphosphate (ATP) which in turn invokes a painful sensation. ATP is broken down into AMP (adenosine monophosphate), which PAP converts into adenosine, a molecule known to suppress pain.[9][10]
History edit
PAP was the first useful serum tumour marker and emerged in the 1940s and 1950s.[6]
See also edit
References edit
- ^ a b c GRCh38: Ensembl release 89: ENSG00000014257 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000032561 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Page 1135-1136 in: Walter F. Boron (2003). Medical Physiology: A Cellular And Molecular Approaoch. Elsevier/Saunders. p. 1300. ISBN 978-1-4160-2328-9.
- ^ a b Taira A, Merrick G, Wallner K, Dattoli M (July 2007). "Reviving the acid phosphatase test for prostate cancer". Oncology (Williston Park, N.Y.). 21 (8): 1003–10. PMID 17715699.
- ^ Genega EM, Hutchinson B, Reuter VE, Gaudin PB (November 2000). "Immunophenotype of high-grade prostatic adenocarcinoma and urothelial carcinoma". Mod. Pathol. 13 (11): 1186–91. doi:10.1038/modpathol.3880220. PMID 11106075.
- ^ Münch J, Rücker E, Ständker L, Adermann K, Goffinet C, Schindler M, Wildum S, Chinnadurai R, Rajan D, Specht A, Giménez-Gallego G, Sánchez PC, Fowler DM, Koulov A, Kelly JW, Mothes W, Grivel JC, Margolis L, Keppler OT, Forssmann WG, Kirchhoff F (2007). "Semen-Derived Amyloid Fibrils Drastically Enhance HIV Infection". Cell. 131 (6): 1059–71. doi:10.1016/j.cell.2007.10.014. PMID 18083097. S2CID 7921205.
- ^ New pain relief that is eight times stronger than morphine, Daily Telegraph
- ^ Zylka MJ, Sowa NA, Taylor-Blake B, et al. (October 2008). "Prostatic acid phosphatase is an ectonucleotidase and suppresses pain by generating adenosine". Neuron. 60 (1): 111–22. doi:10.1016/j.neuron.2008.08.024. PMC 2629077. PMID 18940592.
Further reading edit
- Ostrowski WS, Kuciel R (1994). "Human prostatic acid phosphatase: selected properties and practical applications". Clin. Chim. Acta. 226 (2): 121–9. doi:10.1016/0009-8981(94)90209-7. PMID 7923807.
- Cooper JF, Foti AG, Shank PW (1978). "Radioimmunochemical measurement of bone marrow prostatic acid phosphatase". J. Urol. 119 (3): 392–5. doi:10.1016/S0022-5347(17)57499-6. PMID 76687.
- Cooper JF, Foti A, Herschman H (1979). "Combined serum and bone marrow radioimmunoassays for prostatic acid phosphatase". J. Urol. 122 (4): 498–502. doi:10.1016/S0022-5347(17)56480-0. PMID 480493.
- Sharief FS, Li SS (1992). "Structure of human prostatic acid phosphatase gene". Biochem. Biophys. Res. Commun. 184 (3): 1468–76. doi:10.1016/S0006-291X(05)80048-8. PMID 1375464.
- Nguyen L, Chapdelaine A, Chevalier S (1990). "Prostatic acid phosphatase in serum of patients with prostatic cancer is a specific phosphotyrosine acid phosphatase". Clin. Chem. 36 (8 Pt 1): 1450–5. doi:10.1093/clinchem/36.8.1450. PMID 1696855.
- Kamoshida S, Tsutsumi Y (1990). "Extraprostatic localization of prostatic acid phosphatase and prostate-specific antigen: distribution in cloacogenic glandular epithelium and sex-dependent expression in human anal gland". Hum. Pathol. 21 (11): 1108–11. doi:10.1016/0046-8177(90)90146-V. PMID 1699876.
- Van Etten RL, Davidson R, Stevis PE, et al. (1991). "Covalent structure, disulfide bonding, and identification of reactive surface and active site residues of human prostatic acid phosphatase". J. Biol. Chem. 266 (4): 2313–9. doi:10.1016/S0021-9258(18)52245-6. PMID 1989985.
- Tailor PG, Govindan MV, Patel PC (1990). "Nucleotide sequence of human prostatic acid phosphatase determined from a full-length cDNA clone". Nucleic Acids Res. 18 (16): 4928. doi:10.1093/nar/18.16.4928. PMC 331993. PMID 2395659.
- Warhol MJ, Longtine JA (1985). "The ultrastructural localization of prostatic specific antigen and prostatic acid phosphatase in hyperplastic and neoplastic human prostates". J. Urol. 134 (3): 607–13. doi:10.1016/S0022-5347(17)47311-3. PMID 2411954.
- Sharief FS, Lee H, Leuderman MM, et al. (1989). "Human prostatic acid phosphatase: cDNA cloning, gene mapping and protein sequence homology with lysosomal acid phosphatase". Biochem. Biophys. Res. Commun. 160 (1): 79–86. doi:10.1016/0006-291X(89)91623-9. PMID 2712834.
- Vihko P, Virkkunen P, Henttu P, et al. (1988). "Molecular cloning and sequence analysis of cDNA encoding human prostatic acid phosphatase". FEBS Lett. 236 (2): 275–81. doi:10.1016/0014-5793(88)80037-1. PMID 2842184. S2CID 8445782.
- Yeh LC, Lee AJ, Lee NE, et al. (1988). "Molecular cloning of cDNA for human prostatic acid phosphatase". Gene. 60 (2–3): 191–6. doi:10.1016/0378-1119(87)90227-7. PMID 2965059.
- Sharief FS, Li SS (1994). "Nucleotide sequence of human prostatic acid phosphatase ACPP gene, including seven Alu repeats". Biochem. Mol. Biol. Int. 33 (3): 561–5. PMID 7951074.
- Virkkunen P, Hedberg P, Palvimo JJ, et al. (1994). "Structural comparison of human and rat prostate-specific acid phosphatase genes and their promoters: identification of putative androgen response elements". Biochem. Biophys. Res. Commun. 202 (1): 49–57. doi:10.1006/bbrc.1994.1892. PMID 8037752.
- Banas B, Blaschke D, Fittler F, Hörz W (1994). "Analysis of the promoter of the human prostatic acid phosphatase gene". Biochim. Biophys. Acta. 1217 (2): 188–94. doi:10.1016/0167-4781(94)90033-7. PMID 8110833.
- Ostanin K, Saeed A, Van Etten RL (1994). "Heterologous expression of human prostatic acid phosphatase and site-directed mutagenesis of the enzyme active site". J. Biol. Chem. 269 (12): 8971–8. doi:10.1016/S0021-9258(17)37063-1. PMID 8132635.
- Li SS, Sharief FS (1993). "The prostatic acid phosphatase (ACPP) gene is localized to human chromosome 3q21-q23". Genomics. 17 (3): 765–6. doi:10.1006/geno.1993.1403. PMID 8244395.
- Quintero IB, Araujo CL, Pulkka AE, Wirkkala RS, Herrala AM, Eskelinen EL, Jokitalo E, Hellström PA, Tuominen HJ, Hirvikoski PP, Vihko PT (2007). "Prostatic acid phosphatase is not a prostate specific target" (PDF). Cancer Res. 67 (14): 6549–54. doi:10.1158/0008-5472.CAN-07-1651. PMID 17638863.
- Lindqvist Y, Schneider G, Vihko P (1993). "Three-dimensional structure of rat acid phosphatase in complex with L(+)-tartrate". J. Biol. Chem. 268 (28): 20744–6. doi:10.1016/S0021-9258(19)36845-0. PMID 8407898.
- Darson MF, Pacelli A, Roche P, et al. (1997). "Human glandular kallikrein 2 (hK2) expression in prostatic intraepithelial neoplasia and adenocarcinoma: a novel prostate cancer marker". Urology. 49 (6): 857–62. doi:10.1016/S0090-4295(97)00108-8. PMID 9187691.
External links edit
- prostatic+acid+phosphatase at the U.S. National Library of Medicine Medical Subject Headings (MeSH)